In Memoriam
John Friedberg
In remembrance of Dr. John Friedberg, see below his obituary as well as his personal reflections on his cancer diagnosis and treatment.
Obituary
San Francisco Chronicle
June 10, 2012
Dr. John Mark Friedberg, March 26, 1942 - May 19, 2012
John Friedberg
1964 graduation
Dr. Friedberg died peacefully at his home in the Oakland Hills surrounded by loved ones, after a valiant struggle with kidney cancer.
Born in New York, Dr. Friedberg graduated from Lawrence High School on Long Island, followed by Yale University and University of Rochester School of Medicine. As a Board Certified Neurologist, he was a brilliant diagnostician. He used his keen intellect and sometimes unconventional approaches to build a thriving solo practice in Berkeley that spanned more than three decades.
He was a champion for the underdog, and was well known for his courageous opposition to abuse by the psychiatric establishment. He authored Shock Treatment Is Not Good For Your Brain in 1976.
A polyglot and lifelong learner, Dr. Friedberg had a zest for life and adventure. Outspoken but diplomatic, he loved nothing more than a great debate. A true aesthete, Dr. John chose to live surrounded by beauty; his house and garden was a small paradise with a three-bridge view -- as anyone who spent time in his hot tub can attest.
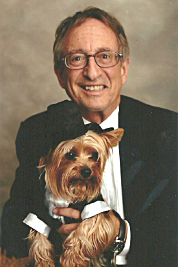
John Friedberg and Buddy
He was a man of many pursuits and passions: an avid gardener, snowboarder, writer, painter, moviemaker, and photographer. He loved entertaining friends with good food and drink and lively conversation. He loved his walks at Ocean Beach and never tired of the wonders of the San Francisco Bay Area.
In 2004, Dr. Friedberg's life was forever changed by the arrival of Buddy, his beloved Yorkshire Terrier. It is rare to find a person who loved his dog as much as Dr. Friedberg loved his Buddy.
Dr. John is survived by his sister, Martha Friedberg, niece Emily Friedberg, brother Robert Friedberg, loyal and loving friends, including Emily Mussi, Bettina Koblick, and Laurel Gray, many colleagues, cousins, countless patients, and fellow Yorkie owners. Special thanks to Robert Nagourney, M.D., of Rational Therapeutics. Donations may be made to The Vanguard Cancer Foundation Trust, Long Beach, CA.The following monograph was published by Dr. Friedberg on the internet. It was last revised on November 6, 2011, six months before his death.
CLOSE CALL
A Doctor's Encounter with Cancer
and The Test That Saved My Life
by
John M. Friedberg, M.D.
Contents
Foreward
Chapter 1: Intimations
Chapter 2: Diagnosis
Chapter 3: Thoracentesis, Sutent, and Sitzkrieg
Chapter 4: Pilgrimage to Long Beach
Chapter 5: Hitting Bottom
Chapter 6: Living on Borrowed Time
Chapter 7:
The Keynote Address
Chapter 8: Tribute to Buddy
Foreword
There are some things we can only experience for ourselves.
Very few who have not had cancer themselves would believe how little is known about treatment and how ineffective most of it is.
As this becomes evident, we are dying. It is too late for most.
In my case, my chest was ravaged by metastatic kidney cancer, my red blood cells were mysteriously gone, and the medication I had obediently taken for three months had done nothing. I was not expected to live.
As a doctor I was accustomed to seeing sensitivity testing and assumed it was done wherever possible. For example, throat swabs are routinely plated on nutrient gels such as agar which are embedded with discs of different antibiotics. The halos of bacterial death around the discs tell us which is the best choice. We do the same for bladder infections. The tests are called "culture and sensitivity" and the words are a medical meme.
Amazingly, culturing cancer cells and testing for sensitivity to cancer drugs are not routine, nor is such testing paid for, and the principled individuals offering such testing are dismissed as "not ready for prime time." As a result of such arrogant dismissals, these obvious and rational tests are almost impossible to locate and obtain in the finite time of a cancer diagnosis.
Good fortune led me to Robert Nagourney, M.D., an oncologist who does drug sensitivity testing on samples of patients' tumors. Just in the nick of time, almost four months after diagnosis, I made a "pilgrimage" in October from my home in Oakland to his office in Long Beach, California.
The test led Dr. Nagourney to recommend three conventional anti-cancer drugs in combination. None of them are drugs of choice for kidney cancer; none of them would have been tried for me.
In two weeks of treatment my chest x-ray, the effusion, the pleural metastases, had cleared dramatically, my blood count was improving, and I was feeling better. As of this writing, ten months after diagnosis and six months on treatment, my chest metastases have "melted away," and my improvement, according to Gary Cecchi, M.D., my local oncologist, is amazing.
The tumor remains, unchanged in size. Surgical removal is an option.
I have no assurance that the army of "renegade immortals," the kidney cancer cells, won't come back tomorrow. I may be living on borrowed time. I am choosing to use it to tell my story because, even though I'm a physician, I suspect my encounter with cancer is not that different from the experience of many others.
Except, perhaps, for the outcome.
The public needs to know about the important work being done by a handful of physicians like Dr. Nagourney who are routinely saving lives with customized cancer therapy.
Chapter 1: Intimations
"You're a doctor — a neurologist — and you ignored hematuria?" (Hematuria is blood in the urine.)
Yes, and smoked cigarettes too. If anything, I thought I'd get lung cancer. Now I'm a doctor with cancer of the kidney.
Two years ago, in a dim State Beach men's room north of Santa Cruz, I peed blood.
Not amber urine or orange or even pink. Red and thick as tomato juice. Later that day, in the toilet bowl, were several delicate corkscrew red spirals, none bigger than a fingernail. They looked at first like worms but were inert and on slight prodding disintegrated into red pigment.
I knew what they were. So much is unchanged since medical school training in the 1960s. They were "casts" and are formed from blood which has leaked and pooled in the smallest kidney tubules, the nephrons.
I also knew that painless blood and casts in the urine often mean kidney disease, if not cancer.
I was so scared I dreamed I was peeing blood.
And as Ambrose Bierce wrote: "Fear has no brains, fear is an idiot." I made the diagnosis of exertional hematuria – temporary bleeding of the kidney from minor recurrent trauma.
Believe it or not, I blamed my little dog Buddy! He is a seven-pound Yorkshire Terrier who can sneeze on command and howl like a wolf among other tricks. For most of his six years he has been my personal trainer, forcing me to do sit-ups with his tug toy each morning after showering.
If motorcycles and marathons can cause blood in the urine, why not sit-ups with a smoker's cough? That's settled. Brilliant. I tried not to think anymore.
I was scared of cancer but, less logically, of penile catheterizations. I'm not only a squeamish doctor but an idiot as well. A simple ultrasound would have discovered the cancerous tumor years ago, when it was small enough to be removed.
Now, it is Stage 4 and, as the writer Christopher Hitchens recently noted regarding his esophageal cancer, "there is no Stage 5."
Lifelong hamburgers, cigarettes since college, and denial since birth notwithstanding, I exercised regularly, took vitamins and anti-oxidants daily, ate happy cows only, and went ballistic when I found high-fructose corn syrup in my Lorna Doone cookies and Progresso tomato-basil soup.
Buddy and I drink home-distilled water. We have an air filter.
I've since learned that cancer of the kidney is an "internist's cancer," meaning it can cause an array of symptoms and elude diagnosis.
In my case, I had developed a tremor. As a neurologist I was pretty sure it wasn't Parkinson's or Benign Essential. It was what golfers call "the yips."
For a year, unpredictably and with great force, my pen would fly off the page. My office manager discretely resolved the problem by using a rubber signature stamp and filling out forms which required cursive.
And for more than a year my heart rate was over 100, day in and day out. I suspected I was self treating with excessive thyroid. I was taking 150 micrograms per day; after testing I backed off to 125.
Excess thyroid might have explained the fast heart rate, the jitters and, the most debilitating symptom of all, the fatigue. But cutting back didn't help. After a year it was all getting worse, especially the fatigue.
Several times a day I would disappear guiltily into my exam room, lie back on my exam table, plunk Buddy on my chest, and fall instantly and deeply asleep.
Maybe it was my age? Somehow I'd reached 68 and it turns out half of all kidney cancer is diagnosed in the 60-80 age range. I didn't consider either age or cancer too seriously. I couldn't feel either one.
I had rarely dealt with anyone else's cancer. Since the advent of brain scans, neurologists are out of the cancer diagnosis loop.
In 30 years as a neurologist in Berkeley, I hadn't missed a day of work, sitting in the same Yale chair, always confident I could find something to do for migraines and multiple sclerosis, and trying to reinvent the wheel for impossible neurologic diseases like amyotrophic lateral sclerosis and Huntington's chorea.
Having been taught that the patient's history, more than lab tests or physical examination, is the basis for diagnosis, I took extensive histories, typing as fast and as long as anyone could talk. Sooner or later the patients themselves suggested the diagnosis. I took special pride in explaining and resolving anxiety by education alone, usually in one visit and without medication.
I remained active in seeking the abolition of electroconvulsive therapy or ECT or plain old shock treatment.
The intentional induction of convulsions has always struck me, a neurologist who treats epilepsy, as harmful. None of my seizure patients ever reported feeling happier after a spell. I regard ECT as a cruel procedure that causes memory loss and brain damage and calls itself treatment. Since publishing an article in the American Journal of Psychiatry (AJP 134:9, September 1977: 1010-1013) and writing a book on the subject, Shock Treatment Is Not Good For Your Brain (San Francisco: Glide Publications, 1976), I've been used as an expert witness and for legislative testimony.
I enjoyed life and when a patient asked if I planned to retire I was nonplussed.
Overall, even as the tumor on my right kidney was growing several pounds, I never thought there was anything wrong with me.
Then in June 2010, my waist went from 34 inches to 37. Nothing fit. Sweat pants slid off. I paraded in the mirror as if pregnant but made a serious effort to lose weight. I skipped meals, increased the sit-ups with Buddy, and went to the club where I could do the treadmill 30 minutes burning away 300 calories three times a week. Right through June I persevered, adding resistance machines and a swim — all to no avail.
Then one day I couldn't catch my breath. Just walking Buddy up a gentle hill I would have to stop walking to catch my breath. And then I would have to stop speaking.
Not wishing to cancel patients, I waited to have a chest X-ray until June 30, 2010, the first day of the Fourth of July holiday. And my last day in denial.
Chapter 2: Diagnosis
The chest x-ray was done in Oakland, at Dr. Stuart London's imaging facility where Buddy charmed the staff with his "square root of nine" trick.
They say that cancer starts many years before when a single cell of the billions of semi-autonomous cells of which we are composed accumulates enough mutations to become "immortal."
This founder cell, this single renegade cell, loses the obligation to kill itself according to a general pact among cells to self-destruct regularly, a process discovered and named "apoptosis" in the 1970's.
This "programmed cell death" can cause a cell to lose it's cell walls, dissolve its own nucleus, and disappear in hours. Over a year, all the cells in our bodies die and are replaced in the process.
Not cancer cells. They go on living and dividing and growing, insidiously at first, usually painlessly. I've seen breast cancer present as multiple painless lumps everywhere underneath the skin. I've seen lung cancer. I was assisting a spinal surgery and the cancer looked like soft tapioca infiltrating nerve roots in the spine. Immortal tapioca!
Dr. London invited me to have a look at my chest x-ray.
There wasn't time for any of Elizabeth Kubler-Ross' stages of grieving, especially the first: denial. My entire right lung was a white-out, filled to the brim with fluid. And the contents of the chest midline called the mediastinum — the heart, trachea and esophagus — were shifted to the left, compromising my left lung as well.
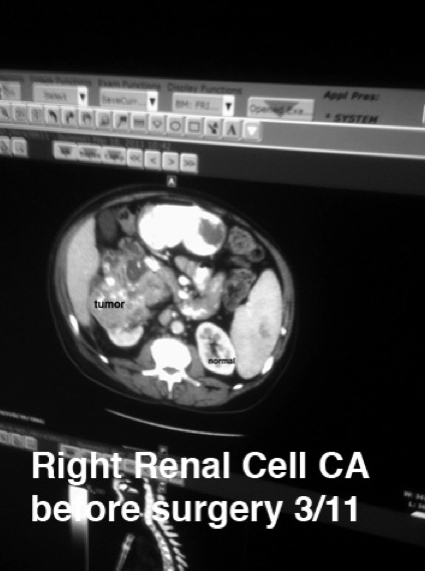
And the cause of the effusion was just as obvious on the ultrasound of my abdomen — a cancerous tumor and a big one: "15 cm heterogenous mass containing internal calcifications arising from the right kidney."
Fifteen centimeters, almost seven inches, is huge. This was not "In situ" or Stage I. My cancer had spread to distant sites including the linings (pleura) of my lungs and lymph nodes up to my neck giving me a statistical chance of one in ten of living five more years.
The prognosis for pancreatic cancer with distant metastases is worse. One in fifty will live five more years.
I learned more bad news from Wikipedia. Solid tumors (as opposed to the leukemias) are the most difficult to treat. Worse, it's medical dogma that kidney cancer is resistant to radiation and chemotherapy.
There are approximately 58,000 new cases of kidney cancer every year in the United States and 13,000 deaths.
I could Google no more. I wanted that tumor out.
Chapter 3: Thoracentesis, Sutent, and Sitzkrieg
Take it out!
My first instinct was to find a surgeon. Like so many, I was skeptical of what chemotherapy could accomplish. And the knife is so intuitive.
And I thought I knew the surgeon who could do the operation: Joseph Presti, M.D. Fifteen years before he had removed a varicocele, a benign but scary overgrowth of veins in the scrotum, and reassured me that I was "too old for testicular cancer."
Surely he was the one to cure my cancer by removing it. He had moved from Mt. Zion Hospital in San Francisco and was now Director of the Urologic Oncology Program at Stanford University School of Medicine.
I faxed and called his office but I never got to talk directly with Dr. Presti. Stanford is highly automated these days.
His office arranged for a state-of-the-art CT scan of my abdomen and chest to be done the next day. After the scans, on Friday July 2, 2010, I was urgently contacted and directed by scheduling clerks and robo-calls to report to Stanford's Interventional Radiology Department immediately.
I had little idea what to expect even as I was being wheeled into the operating room.
Dr. Daniel Sze was an interventional radiologist with a tiger-striped lead apron explained thoracentesis, a procedure for drawing fluid out of the chest which I myself had learned to do in my training. I also remember learning that malignant effusions recur. Dr. Sze said he would be leaving a drain in for recurrent fluid.
The Fentanyl and Versed were a joyful escape. I never felt the insertion of the chest tube and drain. They withdrew over 1300 cc of yellow fluid. I could breathe again.
The pleural fluid was sent to the laboratory for microscopic evaluation: "….cell block sections show malignant cells with nuclear enlargement…..increased N:C ratios….compatible with metastatic carcinoma."
Here too, not much has changed since medical school at Rochester in the 1960's: irregular cells with big nuclei (excessive ratios of the nuclei to cytoplasm or cell fluid) are hallmarks of cancer reflecting excess mutated DNA.
Cancer is "heterogenous" (i.e. composed of unlike substances and structures) under the microscopic and at autopsy: lumpy, bumpy, with dead zones and calcifications. Cancer is ugly.
The drain, referred to as a "pigtail," is also ugly. It consists of a sturdy rubbery tube projecting from the back of my chest. It required daily dressing changes in a location I couldn't reach and never allowed me to forget I was a sick patient.
The drain never drained after the first day, a not uncommon failure.
The other problem, besides my breathing, was severe anemia that had come on insidiously over the same months I was fighting fatigue and a growing belly.
Anemia is measured by hemoglobin (Hgb) levels in the blood. Low normal is usually given as 13.5 mg%. Mine had been normal in April after which some tipping point had been reached and at Stanford it fell to 7.4.
How low can the hemoglobin go? Some sources recommend transfusion when the hemoglobin falls below 12. If an animal were to suddenly bleed out 40% of its blood volume it would cause irreversible shock and death. That was the entire point of the cruelest "dog lab" in medical school.
Severe anemia and lungs full of cancer had a profound effect on my ambition, my energy, and my cognition. I had no objection therefore when, after the thoracentesis, they wheeled me to a room and admitted me to Stanford Hospital.
That night the Pleur-evac Chest Drainage System reservoir overflowed and spilled all over the floor.
House staff over the holiday weekend didn't seem to know why I was there or who my doctor was. They kept asking me "What's the plan?" confirming the old rumor that death rates in teaching hospitals spike over the 4th of July, the traditional annual turnover of house staff.
Over the next two days I was given 4 units of "packed red cells" bringing my Hg to 9.3. I was discharged Monday, July 5th with an appointment for Dr. Presti's clinic the next day to see an oncologist.
I arrived with an entourage including my Renaissance friend Dr. Tom Stern, my super nurse friend, Karen Garrison, my girlfriend Cheryl, and my office manager and now personal assistant, Emily.
Dr. Lauren Harshman, the oncologist, was flanked in the crowded quarters by her two assistants. She wore a fixed smile and a tailored suit. She introduced herself and explained that Dr. Presti would drop in later but he wanted me to start with her. He couldn't just take it out.
"Why not?"
Patiently she explained: "When we know the burden of tumor is systemic we do a couple of cycles of a drug such as Sutent and if there were sufficient shrinkage then we could send you for surgery, maybe two or three months from now."
She took pride in pronouncing the ungainly generic and slick trade names of the new multi-kinase and mTOR inhibitors.
"In the past four or five years there's been an explosion of agents including Sunitinib or Sutent, Sorafinib or Nexavar, and Temsirolimus or Torisel and there's Avastin which inhibits new blood vessels. We're seeing 30 to 40% response rates and stabilization meaning your tumor doesn't grow for 8 to 12 months."
She explained how radiation doesn't work for kidney cancer. Nor does traditional chemotherapy with drugs like cisplatin and 5FU or immunotherapy with the interleukins. They don't work either.
She never used the word cure. She never mentioned survival and there were no success stories. Not a single anecdote. But her smile never faltered. When asked about alternative treatments she explained that she is "an evidence-based doctor."
I asked her what she thought of Andrew Weil, MD, a well known Harvard-educated authority on alternative medicine, and she replied that she was from the East Coast and by the way I should avoid Vitamin C and mushroom extract as these can be damaging to remaining kidney and liver function.
I asked her about turmeric and whether to favor or avoid animal protein or sugar. She laughed nervously but confined her recommendation to a daily multivitamin and, of course, Sutent.
She scheduled me for a cardiac ultrasound because of Sutent's potential for damaging the heart and referred me to a hematologist because she'd only found three reports of kidney cancer causing my degree of anemia. One of her nurses was overheard referring to my tumor as "funky."
Finally she signed me up for a research study — "for the betterment of science" — consisting of sequential positron emission tomography (PET) scans to evaluate the efficacy of Sutent.
The PET scan is helpful in evaluating metastases because it measures glucose utilization and cancer has a big sweet tooth. It also scans the entire body. But PET scans involve radioisotopes and radiation.
I've always mistrusted invisible hazards, especially radiation. I wouldn't let dentists take x-rays. But there I was, twice over the summer, in a trailer plastered with orange and yellow nuclear warnings in a parking lot at Stanford.
Finally, as promised, Dr. Presti popped in. I remembered his sympathetic manner and he remembered the bottle of Glenfiddich "to steady his hand" before the varicocele surgery years ago. But he didn't have good news. Kidney cancers are bloody and difficult to remove and when they've spread, surgery is of no benefit at all. Even the reports that 0.4% of patients experience shrinkage of metastases after removal of the primary are apocryphal.
With his soft words I felt I'd been ushered over the border into "Tumor Town," as Christopher Hitchens calls it. Here people walk around with bruised and bandaged arms. They push IV poles. They speak of odds and percents, of "shrinkage" and "response" and "quality of life" — never "cure."
The denizens of Tumor Town spend much of their time at registration desks and in waiting rooms, at interventional radiology and scanning, receiving transfusions and infusions, standing in queues at pharmacies and failing to get answers to just about anything they remember to ask about when they have the chance to.
"Why am I anemic? Why is my right leg swollen? Am I getting better or worse?"
After that first visit to Stanford's Advanced Cancer Center, the summer was a succession of long commutes, of innumerable little pokes and slight sticks, chest x-rays, CT scans, 6 transfusions, 5 thoracenteses, and multiple doctor visits.
A thoracentesis is a procedure whereby a needle is placed between ribs and into the chest cavity without perforating the lung and causing air to escape from the lung, a complication called pneumothorax. The procedure also carries the potential of infection and hemorrhage but every one of the five I had at Stanford and another at Long Beach Memorial were carried out perfectly.
Unfortunately, with each procedure fewer cubic centimeters of pleural fluid drained and less relief was obtained.
Each of the five procedures took the better part of a day and each thoracentesis involved a radiologist or two, operative personnel, operating room, and medications.
It is eloquent evidence of the Byzantine state of medical billing that Stanford had to charge a total of $21,291.49 for each of the procedures to get paid a grand total of $1977.50 by my insurers, Medicare and Blue Shield.
I don't think the public appreciates how medical prices have been "fixed" for years. I am on Medicare but this is true even for younger patients because, regardless of what the provider (doctor, laboratory or hospital) asks for, Medicare "allows" only a small fraction, pays even less, and "balance-bills" the "medi-gap insurer" if there is one, or the patient, for the difference.
Most private insurers use Medicare's fee schedule — and approved procedures — as benchmarks. The result is inflation of charges and reliance on specialized medical billing professionals, software and computers, overhead which helps drive out the sole proprietors. Only 18% of neurologists are now independent practitioners like I was.
Sutent, a mousy brown capsule, costs $350 per day although after the first week it was subsidized by Pfizer for me as my only income was my monthly Social Security check. I called it my "golden pill" and swallowed with as much ceremony as possible.
I attempted to return to work but found myself winded just getting blood pressures and ankle reflexes. As my gluteus muscles were first to exhibit the still unexplained cancer effect of wasting, or cachexia, I was continuously hoisting my trousers up. I was also back to napping.
I couldn't return to my wonderful practice where patients said good things about me on Yelp and I was making enough money to allocate an hour to each new patient and allocate a generous 30 minutes for each folIow-up visit. I had the luxury of researching what I didn't know and to be an oblivious spendthrift in business and still have enough for a modest contribution to my retirement IRA each year.
Throughout the summer I was increasingly short of breath with any activity including just talking. I prepared my first "Last Will and Testament." I lingered in bed until noon each day and relished doing as little as possible.
The "war on cancer" analogy never seemed apt but this time of waiting, waiting for Sutent to do something, waiting, not for a cure but for "shrinkage," waiting mostly for hope and fearing the next drop of the shoe, the summer of 2010 could aptly be named my sitting down war, my Sitzkrieg, the nervous interval between Hitler's conquest of Poland and his invasion of France.
The internet was a mix of dismal statistics, desperate patients confused about their chemotherapy, and exaggerated promises. I contacted one physician who, for $30,000 and a trip to Manila, would create customized antibodies by mixing my tumor cells with my stem cells, incubating the mix, and injecting them back into me as a vaccine. I didn't buy into it.
To this day, well-meaning friends push the vegan cause insistently until I beg them to stop blaming me. The sub-text of their advice is that I caused my cancer and I was failing to save my life. I point out that blaming the victim is what we do out of ignorance as when the bacterial cause of tuberculosis was unknown and the disease blamed on suppressed passion. I point out that proven nutritional deficiencies are rare — except among certain health faddists. I point out Hitler was a vegetarian. None of my arguments convinced them. None of theirs deter my craving for meat.
However, a scientifically persuasive book, The China Study (2006) by T. Colin Campbell et al is making inroads on my thinking.
My girlfriend shares a wonderful human association of love and food and the instinct to feed disease away. After giving up converting me to raw food, she made the best chicken soup adding mushroom extract and turmeric.
I was nearing the completion of two Sutent cycles: four weeks on, two off.
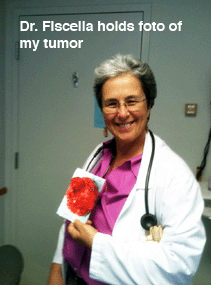
In early September, I asked my primary care physician in Berkeley, Dr. Roxanne Fiscella, to recommend an alternative medicine opinion. She referred me to Michael Broffman, director of the Pine Street Clinic in Marin County, a small Victorian furnished with Asian carpets, Chinese books, and two standard poodles.
Mr. Broffman makes no claim to being a physician. He specializes in cancer counseling. We met in a small cubicle.
"So, do you know anyone who has beaten kidney cancer?" Cancer has made me cut to the chase.
He seemed prepared. He had reviewed his files in preparation for our meeting. He'd counseled over a hundred patients with my diagnosis. And yes, he could think of one man still alive 15 years after moving to Sienna, Italy. Several times a week his blood is circulated through an ozone generator.
As for more practical options, I received an email two days later listing "creative oncology" therapies I could "look into."
These suggestions were numerous. Some were familiar such as low-dose Naltrexone, something I've prescribed at the request of multiple sclerosis patients; some were odd like the cough medicine Noscapine, available by prescription in Israel and Canada. It made me nauseous.
The list went way on — Laktoferritin to protect against iron and Metformin to lower blood sugar and starve the tumor. I liked the Artemissinim, which has the charm of wormword, the prestige of ancient China, and a fine bitterness that comes right through the capsule.
The email included a recommendation for the "Pine Street Chinese Herbal Formula," otherwise unidentified large maroon capsules in a cardboard takeout box. The list included Vitamin D3 and Omega 3 and Super Bio-Cucumin Formula and Medical Marijuana tincture and the following "nutrient sources."
The three page email on September 8 also recommended testing for "iodine loading" and C reactive protein and serum selenium, and although it didn't specify ex vivo chemical sensitivity testing it did list Dr. Nagourney's website under labs: Rational Therapeutics.
The consultation cost and Chinese herbs came to $400 cash and until I got really sick I was taking everything Mr. Broffman recommended that was not illegal or unobtainable or human mother's milk.
But it was the link to Rational Therapeutics that saved my life. The website conveys candor and honesty but the best part was that I was able to speak directly with Robert Nagourney, M.D. the oncologist who has founded and run this combination clinic and laboratory for many years. He was personable, anything but pushy, and had one very good "success story." Above all he made sense. His approach is just what he says it is: rational.
Who would believe oncologists aren't routinely matching the chemotherapy to the individual's cancer?
All Dr. Nagourney needed was a gram of fresh tumor tissue. I had been following a lump in my right armpit that grew from almond to brazil nut on Sutent but I wasn't quite ready to switch my "care" from Stanford.
Stanford's landscaping is a treat for the eye. Their buildings are shiny and clean. On September 21, 2010, a repeat chest x-ray showed "progression" of the disease with "interval development of lymphadenopathy and a large right pleural effusion with loculation and the interval development of a small left subpulmonic effusion."
The word "loculation" is onomatopoetic. It just sounds like sticky strands and entrapped pockets of proeinaceous cancerous gunk and increasingly over the summer and fall loculations were invoked for the diminishing returns from the multiple thoracenteses.
On Friday, September 24, 2010, we went to Stanford for a follow-up PET scan.
This time, just for fun, I brought my Geiger counter. I, who wouldn't let dentists take x-rays, calmly listened as my Geiger counter went off scale and, within a three-foot radius of me, crackled like Krispies for 24 hours.
The report was awful:
"…..increased lymphadenopathy overall worsening with new lytic lesion in lumbar one vertebral body."
Translation: cancerous metastases were taking over my entire lymphatic system and now there was cancer in a spinal bone, portending pain and paralysis.
On September 28, I had my fifth thoracentesis, this time to remove the pigtail entirely. It hadn't drained in weeks.
On that last visit to Stanford's IR department, by another tiny poke of fate, I find out Stanford does electroconvulsive therapy (ECT), the intentional induction of seizures and memory loss and now and then a brain hemorrhage.
Inducing convulsions with electricity is the exact opposite of what neurologists should be doing and mostly what we do. Control seizures. Abolish seizures. It is what our patients want. It is all epileptics have wanted from the dawn of history.
So we mix and match medications, obsess over blood levels, obsess over auras, caffeine intake, quality of sleep. Some patients are sent for surgery just to prevent seizures.
So what kind of doctors induce epilepsy with electricity? Ken Kesey called them shock doctors.
We surge-protect our computers but not our brains? The con is obvious. It has been obvious for 72 years. Shock doctors willfully mis-identify brain damage as improvement. Patients strain to believe them or not. Some rationalize the inevitable amnesia; others resent it.
"They do a lot of shock treatment here," commented the Interventional Radiology nurse wheeling me to the elevator, out of the blue.
"Outpatient shock treatment," she added. "Court ordered."
She was wrestling out loud with her conscience. She was being "blooded," coerced to cooperate and help administer shock treatment. I had seen it before. In her heart she knew it was all wrong.
She could not have known how much I agreed with her.
"I hate it," I said, by way of support: "I've written a book called Shock Treatment is Not Good for Your Brain."
And with that the elevator door opened and closed and we were on our way to the kidney clinic one last time.
I wasn't in a great state of mind: I was coming out of anesthesia, without food since the night before, overall loopy.
Dr. Harshman concluded, after three months on Sutent:
"Your tumor isn't necessarily shrinking; there is a new left neck node; the tumor shows central necrosis, they call it a mixed response; you have this new growth in your vertebra and we can give you Fosamax for that. But there are no lymph nodes in the belly or in the lungs themselves so you might want to continue on Sutent but the mediastinal adenopathy has increased overall and so your disease is increasing so what I would like to do is a biopsy and the next drug I would go to would be an mTOR inhibitor; there can be mouth sores and rash; you can get liver abnormalities and by the way it really makes me nervous, the mushroom extract you're taking. It can damage the liver. And the vitamin C can cause kidney damage. The other option we can biopsy the lymph nodes; and we can give Everolimus, which doesn't have as great a response as Sutent which didn't work at all for you and is one of the most toxic drugs I give but I'd let you stay on the Sutent pending the biopsy."
My Stanford oncologist punctuated this inchoate speech with sharp little raps of her knuckle on my knee. And nervous giggling.
I asked what she thought of Dr. Nagourney's sensitivity testing, matching the tumor against the drug, the better to choose.
She asserted that the test was "not FDA approved." I think she meant it isn't paid for by insurance. Which is true. It cost $3500 out of pocket (now $4000).
I cut a deal with Dr. Harshman: I agree to a redundant biopsy on the single condition that one gram of the tumor be sent to Dr. Nagourney at Rational Therapeutics.
My stalwart office manager provided everyone in our path with a printout of Dr. Nagourney's requirement for a gram of fresh tumor.
They scheduled me for another two units of blood on Saturday, and the biopsy the following week.
Saturday's transfusion at Stanford's transfusion center was Ground Hog Day all over again. It took from 9:30 AM to 10:30 PM for the same reason they'd given the time before: the order for typing and cross-matching hadn't been labeled "stat" in the computer. And my blood was increasingly hard to match. And no one really knew why I was there.
But the biopsy was the last straw. Once again it was scheduled in interventional radiology and at 11:30 AM they had me plugged into an IV, tethered to yet another IV pole, the so-called "Christmas tree." And then nothing happened for 3 hours at which point a radiologist informed everyone that most unexpectedly their CT scan was broken.
I took the opportunity to double check that when their scanner was working again they would be able to send out a gram of tumor for testing.
The radiologist was uncertain. Her colleague who was summoned had no doubt: neither the Fine Needle Aspiration nor the Core Needle Biopsy could yield a gram of tissue.
"You would need a hundred — well at least ten sticks."
Reportedly I left "hollering and cursing."
I was done with Stanford. I would go to Long Beach. I called Long Beach as we were pulling out of the parking lot.
The clock was really ticking now. I was gasping like a fish out of water. The CT scan and the PET scan were both worse and my oncologist had no better ideas than redundant biopsies, more Sutent, or switch to something even less likely to work.
I needed a booster shot of hope and I got it with my "pilgrimage" to Long Beach.
Chapter 4: Pilgrimage to Long Beach
The trip to Long Beach felt like my last chance. Stanford had failed me. The fiasco with the "biopsy" was the last straw but it was the proven failure of the Sutent that demanded I try something new.
Monday, October 11, 2010: There was a sense of destiny and deadline. This trip might be my last.
My office manager found day care for her kids and did the driving. She had never been to southern California so after making good time to Los Angeles down Interstate 5 we detoured west to the Santa Monica pier and Venice Beach.
The rings are still there. They dangle from a tall frame over the sand, maybe a dozen rings spaced just right for an athlete to swing from one to the next, turn around and come back, never touching the sand, getting up a rhythm, like Tarzan.
I did that once. No longer. Not today.
My office manager took a swim in the Pacific Ocean while I watched from the beach, saving my breath.

We found the medical suite and lab across the street from a dozen oil wells pumping, and at 11:00 the next morning we met Dr. Nagourney, and he is no disappointment.
His shaved head, concentrated gaze, and suspenders lend a whiff of the wizard.
After an old-fashioned and thorough physical examination he summarized his point of view about cancer: "Cancer cells don't grow too much: they die too little."
Dr. Nagourney compares apoptosis and the other methods of programmed cell death, to the Samurai practice of bushido or ritual suicide. His emphasis is not on cell overgrowth and proliferation — the focus of previous approaches to testing.
Rather: "Our assays look at markers for programmed cell death."
After carefully mixing sufficient fresh tumor material (plus stroma-vessels, connective cells) with various selected cancer drugs in a culture medium, he looks at markers of cell death, or apoptosis.
For example, life is energy. ATP is the biologic energy battery that stockpiles and distributes energy in all cells. Failing ATP, synthesis is made visible by waning photoluminescence made possible in turn by a firefly enzyme aptly called Luciferase.
Another marker is early disintegration of tumor cell walls visualized as progressive failure to pick up certain vital stains.
Impeccable laboratory technique is used to preserve not only tumor cells but bits of the tumor matrix — the capillaries and connective tissue that come with a good sized biopsy.
I was able to see Dr. Nagourney's lab. It is directly adjacent to his exam and consult suite.
I love labs even though I was never very good in them. My "unknowns" so often became "non-existents" but having been educated to do my own urinalyses and even complete blood counts, to look at biopsy specimens and spinal fluid under the microscope, I am in awe of someone with their own lab. I like that Dr. Nagourney was a chemistry major as an undergraduate before he getting his M.D. at McGill University.
"Preserving the matrix" means getting enough tissue to begin with. To me it was logical to take the conspicuously enlarging lump in my right armpit.
It is ironic that the Stanford people projected contempt for "excisional biopsy" as "old fashioned" in relation to their CT-guided fine-needle biopsies and cores.
And an excisional biopsy was just what Dr. Nagourney arranged for that very afternoon with Dr. Azaren at Long Beach Memorial Hospital.
He even worked in another thoracentesis as my breathing was pretty bad. All in one day. All scheduled by telephone. By the doctor himself.
As we left Dr. Nagourney's medical suite, we passed a man coming in holding complimentary tickets. He quickly guessed why I was there and politely turned and followed us out to say that Dr. Nagourney saved his wife's life. More than two years ago she'd been given six weeks to live. She'd seen multiple doctors. Presently she is doing well and her husband is deeply grateful.
It's not only patients who admire Dr. Nagourney. A colleague, friend, and competitor Dr. Larry Weisenthal, on his website has this to say about him:
"Dr. Nagourney uses one of the same core technologies which are used by the Weisenthal Cancer Group, namely the DISC assay (described above), which Dr. Nagourney refers to as the "Ex Vivo Apoptosis Assay" or "EVA." Nagourney's work is quite good and I recommend his laboratory as the first alternative to our own. Comparing and contrasting "us" with "them," I spend full time doing the assays, while Dr. Nagourney maintains a clinical oncology practice, and so is more part-time in the lab. We use more assay endpoints, which I think is advantageous for a number of reasons. I consider Dr. Nagourney, however, to be the best in the world with respect to taking assay results (either ours or his own) and using the laboratory results to design a custom-tailored treatment regimen for an individual patient. When a very close family member of mine needed "custom chemo," we did the testing and gave Dr. Nagourney the results to use in designing and administering an innovative (and successful) treatment regimen. I often refer to Robert as being one of the 10 smartest and 10 most idealistic people I've ever met in my life. That pretty much describes him and his work."
From the moment we accomplished our mission and began our return drive to the East Bay, my memory started giving out. I've been told I spent the drive back reading aloud from Customized Cancer Treatment, a book by Ralph Moss Ph.D. that covers the history of cancer chemo-sensitivity testing. My recollection is patchy and when I re-read the book recently it was like new.
According to my second reading of Ralph Moss, one reason chemo-sensitivity testing isn't routinely done or even mentioned to patients relates to an older method of cloning tumor cells which was perhaps overly hyped and unreliable. As a result of several influential editorials and articles in the 1980's, all testing was shunned because of technical problems growing and testing clumps of tumor cells in what was the "clonogenic" method to evaluate proliferation. This method, on the edge of acceptance — including reimbursement — in 1979, went into eclipse, or, as the author put it: "Within five years the clonogenic assay was brought low and with it went the credibility of the concept of chemo-sensitivity testing as a whole."
Another reason may be the financial interests of academic oncologists in big-money grants from charitable organizations and government to support random-control trials: prestigious, expensive, endless, and often inconclusive.
I myself am unexpectedly grateful to the pharmaceutical companies for making and marketing the drugs that are saving my life and I see no reason they wouldn't want to streamline the selection of new cancer drugs. Dr. Nagourney "partners" with drug companies to do just that.
From that return trip to Oakland and for the next six weeks in the hospital, a concatenation of anemia and lung damage and cancer and drugs produced a low-grade delirium. Delirium is a perfectly good neurologic word meaning organically based confusion and amnesia. That was me on morphine. I am left with memory gaps and not just for the Customized Cancer Treatment book.
Needless to say, it is a challenge to write a memoir about amnesia, almost a contradiction in terms. For the end of October and beginning of November, I have had to piece together written records and the recollections of others.
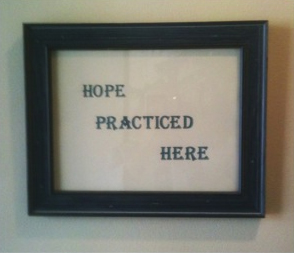
Sign in the waiting room of
Rational Therapeutics
By the time I was back home from Long Beach, I have no recollection at all of dancing naked around the house singing.
My last recollection is seeing my father's elderly face bouncing around on the large IMac screen like a screensaver. And then I realized I was staring at my own reflection. My face was his. It was a most happy delirium thanks to the booster shot of hope I got in Long Beach.
Since I've been home I've received a hundred heartfelt cards and letters including this famous verse from the poem by Emily Dickinson:
HOPE IS THE THING WITH FEATHERS
Hope is the thing with feathers
That perches in the soul
And sings the tune without words
And never stops at all.
Chapter 5: Hitting Bottom
I awoke the very next morning to the strong fear of death and the energy of a burnt-out bulb.
Thursday, October 14, 2010. Admission day.
Short of breath, unable even to stand, I called my girlfriend and she took me to the Emergency Room at Alta Bates Hospital in Berkeley. This was "my" hospital for thirty years, my office was across the street. But it was the last place I wanted to be, under the noses of colleagues. But there I was and there I remained for the next five weeks. From the outset I had no choice about anything and a very scrambled recollection for the duration. I just went limp. Other than to the repeated and increasingly painful phlebotomies, the "little pokes," I objected little. The CT of my chest made an impression on everyone and resulted in a direct admission to the Intensive Care Unit on the pulmonary service. The CT report reads like the battle of Verdun - the largest deadliest battle ever:
"Large loculated right pleural effusion with multiple thick-walled loculations resulting in marked right-lung volume loss. There is a large collection of fluid within the interlobar fissure causing a pseudotumor appearance. ...There is a resultant shift of heart mediastinum to the left with marked atelectasis of the left lung and a freely layering left pleural effusion. Extensive mediastinal and right hilar adenopathy."
In simple English, my right lung was so full of cancerous fluid called a "malignant effusion" that it was crushing the left lung.
And that was just my chest. The primary right kidney cancer was still in my abdomen and there were metastases along the chain of lymph nodes up to my right armpit and my neck. My defenses were overrun.
"Everyone thought you were going to die," I've been told.
In addition to the breathing problem I was severely anemic again.
The Alta Bates blood bank had even more problems with my blood than Stanford. It took the latter 12 hours to cross-match my blood; Alta Bates couldn't do it at all. This meant that I would have to be given unmatched blood, a big "no-no" drilled into medical professionals for a century. But I needed blood.
That was one reason they wanted me in the ICU, to observe the transfusions and resuscitate me in a timely manner.
For three consecutive days after admission I received a unit of packed red cells each day, with hours of pre-medication infusions including IVIG (immuno-globulins from pooled human serum) and steroids and albumin, and an anti-histamine and Tylenol.
Even if I had the strength to move, which I didn't, the logistics of the treatment required immobility. I felt like a float in a Macy's parade. I was on my back in bed, too weak to sit up or even push back, and tethered to the "Christmas tree" by more lines than Gulliver. I didn't move. I had one IV for blood and another for medications; I had a Foley catheter and compression stockings for my swollen calves and oxygen by nasal prongs. I had the call button. I had the morphine button.
They brought food but I had no appetite from the constipation of inactivity, the opiates, and no doubt the "cachexia" of the cancer itself.
The cancer had clearly reached progression stage. My belly grew visibly from day to day. It was "like a Stephen King movie" I've been told. I was oblivious.
I was also losing weight. It didn't help that the food was monotonous and my tastes perverse. All the breakfast I ate for weeks were "pork" sausages doused in "maple syrup."
I had weird stomach aches. An ultrasound was negative for ascites, cancerous fluid.
I begged for enemas, the only thing that worked but labor-intensive and otherwise slightly repugnant to most staff. Moreover, enemas required a doctor's order which involved disturbing the doctor and this didn't always happen.
The constipation was mostly due to the morphine, but the morphine was my only pleasure in life at the time.
It was delivered by PCA, or patient-controlled analgesia. Each time I pressed a button I was rewarded with a reassuring "beep" and two mgs of morphine. The machine would "lock out" at 10 mg per hour but I never needed that much. I used it for escape and it made no difference if I told the nurse my pain was 0 or 10 — I got it anyway.
Most of the time, I wasn't in pain at all. I also had Lorazepam or Ativan, a muscle relaxant, Ambien for sleep, and even a Fentanyl patch, and truth be told, anything else my heart desired! The doctors were utterly compliant with medication requests and nurses never raised an eyebrow. Cancer has its perks. For over a month, day and night, I floated in a twilight state.
Morphine, a "touch of the poppy," makes everything easier: breathing, staying put, passing time. Morphine causes visual hallucinations. I didn't mind the hallucinations, the shadowy rats in my periphery, the faces in the bedfolds.
I found myself listening intensely to my own breathing, expecting a message. With my chest full of fluid, my breathing was a medley of wheezing and wet crepitus like alien Morse code.
Morpheus is the Roman god of dreams. Morphine helped me sleep.
Except one night it seemed I was up all night. It appeared to me that the walls were gray metallic bulkheads and they came together in a point. I stared and stared and realized I was in the prow of a ship. Up and down the China coast we sailed. I'd been kidnapped by the international kidney trade. I knew if I complained to my nurse, that my one good kidney would be gone.
Insomnia and hallucinations at night, talking in my sleep during the day. My office manager recorded some of these articulations on her laptop, verbatim:
"There is an overlap between dogs and their owners."
"Why don't we drag this down the street and see what happens?"
"Intrigued. Um. Ummm. Inside the head you can get temperatures three to four degrees higher."
"Part of the consequence of aging is we lose some of our functional abilities to relate, to relate to other older folks. We can talk about that."
"That is my new girlfriend. Don't you just want to hit her over the head with a rock sometimes?"
"I've got too much drugs."
"It's weird how things have changed. I used to be so scared of cancer images. Things are good."
In the event, things were good.
Three days after my admission to the hospital, even as I was "circling the drain," my cell phone rang. It was Dr. Nagourney. In five days he already had results. There is nothing hazy or distorted in my recollection of his words. He wasn't effusive but he didn't hide his satisfaction.
"Your cancer is resistant to most of the drugs we tested. But it is sensitive to three of them. You could take them together in low doses. You won't lose your hair."
The written report, which followed, was equally straightforward.
The assay quality was "high yield, moderate viability" and after "mechanical and enzymatic degradation" 16 different drugs were tested for the induction of cell death.
The report concludes in bolded type: "Ex Vivo best regimen would be Cisplatin plus Gemcitabine plus Xeloda."
These are three deeply poisonous, well established chemotherapy agents which never would have been recommended by current standards of treatment for kidney cancer.
Cisplatin, introduced in 1965, now relatively inexpensive, interferes with gene replication in the nuclei of cells by cross-linking DNA.
Gemcitabine (trade name Gemzar), a non-functional analogue of a nucleoside, one of the building blocks of DNA, also interferes with a crucial step in the cell cycle — the replication of DNA.
Cisplatin and Gemcitabine must be given intravenously and flushed out immediately which means a day hooked up to IV's. Xeloda or Cepacitabine, the newest and most expensive of the three, is a pill taken twice a day by mouth, two weeks on, one off. It is a pro-drug which converts to an old drug, 5-fluorouracil in the body. It too interferes with DNA synthesis.
All three accelerate apoptosis in cancer cells. And rapidly-dividing normal cells as well. The bone marrow is consistently suppressed and must be stimulated to keep up red- and white-cell production.
Cancer can develop resistance to drugs. Mutation is what cancer does for a living.
I would need an oncologist at Alta Bates to oversee the administration of these drugs, none of which is without risk. Cisplatin in particular can cause kidney damage and deafness. It must be flushed from the system with intravenous fluids and water pills, in my case Lasix and Mannitol.
As any nurse will tell you, getting a doctor to go along with another doctor can be problematic.
Dr. Fiscella visited me in the hospital. She had recommended Mr. Broffman who led me to Dr. Nagourney, and now she made another fortuitous recommendation for an oncologist.
Dr. Gary Cecchi had been a friendly face for thirty years. We were on the education committee together. We seemed to share contempt for the same things although we'd never spoken of what. He has a very active oncology practice in two locations with a staff of nurses and assistants. He also has a winery and a private plane.
I begged him to speak with Dr. Nagourney.
To his eternal credit, Dr. Cecchi came through.
"I spoke with your guy in Long Beach. Good man. None of his three drugs is unconventional. They just wouldn't be considered for kidney cancer. I have no problem giving them."
Gary doesn't talk very much although his sardonic smile suggests lively inner conversation. He did add, quite sincerely, "I'm sorry for what you have to go through."
The tumor was consuming my red blood cells voraciously.
On admission my hemoglobin was 7.7 grams per 100 cc's (g/dl) and 6.5 the next day, less than half the low normal of 13.5. No one seemed to know just how low this number can go but the cutoff for transfusion for me was 8.0. Over the summer I had already been given 10 units of packed red cells at Stanford.
And no one seemed to know what was causing my anemia although hemolysis — rupture of red blood cells — was the best guess. For the first three days at Alta Bates I got a unit of blood each day with roughly a one-point increase for each unit, only to have the Hg drop to 5.8 a week later.
The pre-medications and lymphatic obstruction probably explained my fluid retention. My legs were swollen to the waist like elephantiasis. The right leg, especially, was obscenely bloated and red as a lobster, an asymmetry that defied diagnosis but got a lot of attention from the staff. Two ultrasounds for deep-vein thrombosis were both negative.
During that first week I underwent a thoracotomy for removal of the loculations and pleural metastases on the right. This was not done by the ubiquitous interventional radiologists. This time a venerable and compassionate thoracic surgeon, Dr. Robert Stallone, created a scimitar entry along the right sixth rib large enough as he explained it to stick his hand in and scoop out the cancer.
I like surgeons and the anesthesia that makes it possible for them to do what they do.
The following day I underwent a portacath placement, a sterile reservoir under the skin of my upper chest from which blood could be drawn without more poking and into which medications, specifically the chemotherapy, could be injected. My first chemotherapy treatment on October 20, 2010, was anti-climactic. It only took minutes to inject the Cisplatin and Gemzar. Two specialized oncology nurses in eye-stabbing yellow paper gowns and heavy blue gloves oversaw the administration. With the gravitas of missile launch officers they double-checked my identity, by wrist band and interrogation.
There was less ceremony surrounding the oral medication. Xeloda is a pill taken orally twice a day.
After the infusion of the Cisplatin and Gemzar, the nurses immediately hung bags of sterile saline mixed with Lasix, a powerful diuretic especially when given intravenously. Every hour, all night long, I would claw up out of the deepest sleep to hit the call button. As I had fallen once or twice, a sign on the wall reminded me to "Call Don't Fall." I was pretty close to death although nobody told me that. There was a tendency for my friends to say I looked "better than last time" which I never understood.
I had amnestic interludes. Witnesses tell me I had nausea and dry heaves from the chemotherapy and had to be given Zofran and Reglan but I recall no side effects at all. You would think protracted vomiting would stick in my mind. Much less the devotion of friends who spent the night.
But my mind was elsewhere. I dreamt I had lost my wonder dog. He'd wandered away from me at the Gare du Nord, the North Station, in Paris. We had been inseparable for 6 years. He licked my eyes and nose each morning, came to work and greeted patients, and showed off his mathematical skills by calculating the square root of 9 by pawing three times. At day's end he'd pull off my socks. I missed him so much. Nothing made me weepier than thinking I might not see my funny-face Yorkie again. I wondered if he dreamt of losing me?
He was staying across the street from our house with our generous friend and neighbor Bettina and her Biewer Yorkie Dolce. Reportedly, he waited by Bettina's door for awhile and then proceeded to have a great time dominating the larger dog, Dolce.
I had mixed feelings about him visiting me in the hospital. What if I didn't make it? The staff had mixed feelings about dogs on the unit, period. Three times we got him in and his excitement made it clear he hadn't forgotten me.
A week after my first chemotherapy treatment I got a second. My hemoglobin was back down to a low of 6.1. I received two more units of blood. There was a slight improvement in my breathing after the chest tube was in place, but just barely. My energy was a barely palpable commodity.
I was amazingly passive, content to stare at the television. The cable package had to be the cheapest offering: a choice of Fox News, crime shows, and the Food Channel. Even with all the drugs, it was impossible sleep without interruption. The infusion alarm went off, waking me frequently, when the morphine ran out or an air bubble blocked the line or just for the hell of it.

My day began — or my insomnia ended — at 5:00 am when a technician entered my room to draw blood. Then there were three "evaluations" each day with the nurses' shift changes. They checked my temperature and blood pressure, which were stable. But my weight fluctuated wildly as I bloated and shrank with volume expanders and diuretics.
The skin of my swollen right leg especially was stretched so thin it looked like a bright red blood sausage and it peeled. An infectious disease specialist put me on one antibiotic and then another but the swelling didn't abate and the peeling continued.
Respiratory therapy dropped in twice a day, and dietary personnel with menus of the same foods as last week. And, without knocking, at least four different flavors of uninvited chaplain showed up, including a female rabbi with a wispy beard. They were all upbeat about death.
Some of my friends even spent the night on fold-up beds and shared the hourly interruptions of sleep when the morphine alarm went off or IV bags needed changing or I needed assistance to "stand and pee."
At the very nadir of all this we found a neurologist interested in buying my practice. I had to sell it because my landlord wasn't going to waive the monthly rent of $2800 for the two years left in the lease "unless you're dead."
To get out of a lease I signed without reading years ago, I sold a thirty-year practice for the buyer's assumption of the lease and $100. To the end, I was never much of a businessman.
By October 28, 2010, just after the second infusion of Cisplatin and Gemzar and two weeks of daily oral Xeloda, I was weaker, wasted, and more breathless. My weight was down from 160 to 140, I lost all desire to eat, and I was unable to sit up, shave, or shower. My chest x-ray
revealed deterioration:
"extensive pleural and parenchymal disease ... probably increased."
One of my nurses somewhat cryptically offered: "Let me know if you can't take it anymore."
Out of character, I made myself "DNR" – do not resuscitate. I quickly changed my mind. If there was one thing I had learned in my years as a doctor, it was the difficulty of predicting the time of a patient's death. It is usually best not to hasten the end. Years ago I even wore a dog chain ID which read: "Keep me alive. Spare no expense."
And then something happened, almost imperceptibly at first, then unmistakably: I was getting better and better, fast.
A chest X-ray on November 8, 2010, showed dramatic improvement although we all failed to notice at first. I had to ask the respiratory therapist what it showed. The radiologist reported:
"When compared with a prior chest x-ray of October 21 ... Significant interval improved aeration (inflation with air) …"
It was precisely during this interval that I completed my first two-week cycle of the three-drug regimen recommended by Dr. Nagourney.

The other marker of improvement was my hemolytic anemia. After the last of three units of blood at the end of October my hemoglobins no longer dropped like a stone within days of transfusion. Of the total 17 units of blood I received at Alta Bates, all but three were in October, in other words before starting the chemotherapy.
Best of all I was tentatively coming back to life. I could breathe better. I had more energy and ambition. I actually wanted to take a shower, brush my teeth, change my hospital gown, and eat.
And of course I wanted to visit with my Yorkie pal, Buddy.
By mid-November I was back from the brink. Dr. Cecchi, a man of few words, confessed to being impressed:
"Congratulations," he said.
Looking me in the eye and referring to Dr. Nagourney's recipe he added emphatically: "He nailed it."
I went home on November 19, 2010.
Chapter 6: Living on Borrowed Time
Most of my life there was nothing wrong with me.
I was Peter Pan and I lived in Shangri La with my little dog Buddy.
I once came down KT22, Squaw Valley's original black-diamond run, on my snowboard under the lift-line holding Buddy in my arms. And in my work I followed the advice of Zen master and founder of San Francisco's Zen center to "burn yourself up completely in everything you do."
Time flew by.
Suzuki died of cancer.
Cancer is a scary word. It is more than a death sentence or synonym for death. It is treason to the proud flesh, an affront to ourselves who, as the Bard put it, are "so like the gods."
I remember the plot of a 1950's horror comic I read as a child. A cancer victim somehow contrives to live forever. Unfortunately the cancer lives forever too and quickly consumes the victim who is now a pullulating mass of formless flesh, so ugly he must hide forever in the depth of a cave. That was one scary comic book.
Since my diagnosis I have stumbled down paths of frequently-asked questions no doubt familiar to many others.
For example, does everyone always die from cancer? Does anyone really beat "the big C"?
In 1992 The Institute of Noetics "assembled the largest reported database of medically reported cases of spontaneous remission in the world, with more than 3500 references ..."
The researchers sadly concede such occurrences are "relatively rare."
I came across the depressing apparent paradox of "response without improved survival." I now believe this is a purely statistical conclusion based on averaging. There have been robust remissions lasting many years when the right treatment was chosen.
I know Dr. Nagourney's test and prescription saved my life. I know it extended my life. What's the difference?
I went for a CT scan on January 3, 2011, and spoke with the radiologist by phone: "Everything has gotten better."
The cancerous nodes in my chest were "melting away" and the tumor now measures 12x11x11 centimeters, having previously measured 13.1x13.6 cm before chemotherapy.
Dr. Cecchi used the word "amazing" and compared the dramatic improvement to the favorable responses of some lymphomas.
My own lifespan is already longer thanks to Dr. Nagourney's customized chemotherapy. It's the reason I'm alive to write this. Whatever happens from now on, my experience as related here speaks for itself.
Just as I was finishing this memoir I discovered that Dr. Nagourney wrote about my case on his blog of January 6, 2011:
Are New Cancer Drugs Always Better?
by Robert Nagourney M.D.
Few cancers instill a greater sense of fear in the medical oncologist that metastatic renal cell carcinoma, the most common form of which is known as clear-cell cancer. This type of kidney cancer — driven by a mutation in a gene know as VHL — spreads rapidly, metastasizes to almost any and all organs, and historically responds to almost no therapies. The development of Interleukin-2 (IL-2) in the 1980s offered a glimmer of hope. Yet even this breakthrough ultimately yielded complete and durable responses in a mere 10 percent of patients.
By focusing on the hyper-vascular nature of this disease, investigators then developed a second line of defense that attacked the blood supply of these cancers. Following the introduction of Avastin, a number of small molecule VEGF inhibitors were introduced. Most recently, a class of drugs known as mTOR inhibitors gained popularity by providing objective responses and showing evidence of improved survival.
But what happens when all the really "hot new drugs" fail to provide benefit?
This was a question I confronted in a charming, 68-year-old neurologist who traveled to visit me from Stanford University where he received highly appropriate, yet unfortunately ineffective, therapy. The patient presented in July 2010 with rapidly progressive kidney cancer that had overtaken his lungs. He was started on oral Sutent (the treatment of choice). His management was complicated by a hemolytic anemia. When I met the patient in October, I was concerned that he could not survive long enough to take on another treatment, no matter how effective it might ultimately prove to be.
As a physician, he beseeched me to study his tumor in the hope of finding any therapy to salvage him from his rapidly deteriorating course. A small biopsy was obtained with the help of one of our surgical colleagues. The results were striking — no evidence of activity for sorafenib, sunitinib (Sutent), nor the Rapalogs (Rapamycin derivatives). In one fell swoop, all of the newest therapies were swept aside with little likelihood of benefit. Despite the established literature, this patient was clearly sensitive to chemotherapeutics. It was evident to me that the treatment outline, a combination of three drugs, could provide meaningful clinical benefit if the patient could tolerate even the most modest associated side effects. With the kind cooperation of the treating physician in Northern California, our recipe was followed to a T.
The treating oncologist pulled no punches in his description of this patient's prognosis. Nonetheless, he kindly assisted in the management of the treatment we described. While the cancer-related hemolytic anemia raged, and the patient fought for air, the treatments were delivered. Too ill to leave the hospital, his entire first course of therapy was delivered on an inpatient basis.
For several weeks, we anticipated the worst. And then, a phone call from a chipper-sounding patient. Breathing comfortable, his chest x-ray had cleared, his anemia had resolved, and he was being readied for discharge. A short time later, an abdominal ultrasound revealed measurable improvement in the kidney cancer, further confirming objective response.
The patient, now home, could not be happier. The excellent outcome is as gratifying as it is unexpected. There is no question that no one else would have given this treatment. And there is further no question that the patient would not be alive today had he not received it. There are many lessons to be learned from this experience. Among them, that every patient deserves the opportunity to get better; that laboratory analyses can identify unexpected options for patients, even with the worst malignancies; that new drugs aren't always better drugs; and finally, that nothing succeeds like success."
I've lost 20 pounds which can be a good thing. Everything fits. My girlfriend calls me her "little miracle" and is jealous of my flat abdomen.
My energy is low from chemotherapy and I remain anemic. I spend one day a week getting intravenous chemotherapy. Then, to counteract the effects of the chemotherapy, I require injections of Procrit to build red cells and Neulasta to build white cells.

But now for the first time my doctors are seriously talking about the possibility of removing the tumor. For the moment I am normal. I have a life. I can go snowboarding with Buddy.
I needed to put this account in words for my own accommodation and because I want the most possible people, those to whom it may concern directly and those who care about them, to know about chemo-sensitivity testing. As Dr. Nagourney has written: "Every patient deserve the opportunity to get better."
If we live long enough, cancer will be a concern for 40% of us living in the United States.
From my point of view Seneca had it right:
debilem facito manu,
debilem pede coxo,
tuber adstrue gibberum,
lubricos quate dentes:
vita dum superest, benest;
Epistularum Moralum
Liber XVII
Roughly translated by me: "Cripple my hand, my foot, my hip — knock out my teeth: life is still the greatest good."
I'll toast to "L'Chaim" — to life.
Written March 27, 2011.

P.S. I did have a life before cancer.
Much of my life before cancer is included on Dr. John's Cybersuite, a website I began in 1995 when the first web browser — Netscape — became available. [Webmaster's note: This website is now defunct, as of Nov. 2012.]
Like so many smitten by the internet, I threw privacy to the winds.
Since 9/11, privacy and other rights are eroding fast and the internet has become a two-edged sword. I sort of stopped sharing until I had no choice but to share my good fortune when chemo-sensitivity testing for cancer treatment saved my life.
My old website, touching on dozens of subjects, from neurology to snowboarding to my (negative) opinion of shock treatment and capital punishment to my translation of Casanova's Great Escape, that old hand-made "cob-website" lives on, way too unwieldy to change.
Please visit Dr. John's Cybersuite.
I will be updating the past six months in detail shortly but in May the kidney plus tumor came out and in July my PET/CT was negative.
As of this writing, October 11, 2011, I feel fine. I am anemic from ongoing chemotherapy with my last Hemoglobin 9.4 but anemia is the new normal for me. I also have a prickly but not painful peripheral neuropathy from the platinum which only bothers me at night.
I work out, and I was recently honored to be asked to give the keynote address at the annual Vanguard Cancer Foundation fundraiser in Los Angeles on October 1. It was a very happy event.
Chapter 7: The Keynote Address
VANGUARD CANCER FOUNDATION
Keynote Address
October 1, 2011 in Honor of Robert Nagourney, M.D.
by JOHN M. FRIEDBERG, M.D.
 I want to thank Dr. Robert Nagourney, his office manager Shari Burt, and his entire staff for being asked to speak tonight. I want to thank them for being here at all.
I want to thank Dr. Robert Nagourney, his office manager Shari Burt, and his entire staff for being asked to speak tonight. I want to thank them for being here at all.
I mean on the planet.
I was last here in the Los Angeles area a year ago, on October 13, 2010 to be exact. I was here to see Dr. Robert Nagourney. It was a last-ditch trip.
The day after I got back to my home in Oakland, with my biopsy in his lab, I collapsed and was hospitalized for the next six weeks. I was not expected to live.
The title of my story online is Close Call – A Doctor's Encounter with Cancer and the Test That Saved His Life.
Everyone has a cancer story but mine is a bit of a humdinger. My kidney tumor was so big that when I emailed a photograph of it to a nurse anesthetist and witty friend she immediately emailed back: "Is it a boy or a girl?"
When I last set eyes on Dr Nagourney I was, to use a term of trade, circling the drain.
I had been diagnosed with inoperable metastatic kidney cancer at the beginning of July and despite six blood transfusions, 5 procedures to remove fluid from my chest, and despite my faithful use of Sutent or sunitinib for three months, despite the best efforts of Stanford's Cancer Institute and my oncologist, despite all of that I was closer to death than ever.
I couldn't breathe.
I was losing weight and shrinking, one observer said, "like in a Steven King movie."
 The tumor was 4.7 inches and growing.
The tumor was 4.7 inches and growing.
I am a physician myself, but as a neurologist I knew little about cancer and less about the world of oncology. My primary care doctor, Roxanne Fiscella, referred me to Michael Broffman, a cancer counselor at the Pine Street Clinic in San Anselmo in Marin County.
It was on the third page of his diligent listing of cancer-fighting alternatives that I found the Rational Therapy website listed without fanfare under "labs."
I reviewed the website and it was exactly what it's called: rational treatment.
But when I asked my Stanford oncologist about what I will hereafter refer to as "The Test" (credit to Ralph Moss, Ph.D. — his book Customized Cancer Treatment 2010 is the best book on the subject), she had a knee-jerk response and as a neurologist I'm trained to recognize knee jerks:
"Predictive testing is not FDA approved ..." and that was all she had to say about it.
Other cancer patients like myself have been discouraged by other knee jerks such as "unproven in controlled studies" and "it isn't ready for prime time" which is simply untrue as so many here tonight can attest.
But let me digress for a moment.
There is a disease, bacterial endocarditis, in which microbes can destroy a heart valve in days or even hours. When suspected, the first and most famous order any doctor can give is: "Culture and sensitivity! Stat! "
Bacterial endocarditis is curable if the right antibiotic is chosen based on a bacterial culture and sensitivity test.
No one would be dumb enough to start an antibiotic without a predictive test first.
And yet from the best I can tell, oncologists choose the drugs they administer today by herd instinct, with maybe a touch of black magic and the financially feasible.
Not on what available drug would work best for my cancer or yours.
How can this be? First of all, the wisest men and women make mistakes, sometimes over and over.
I actually made a humdinger two years ago when I ignored blood in my urine. I actually blamed my seven-pound Yorkshire Terrier, Buddy, for pushing the sit-ups too aggressively. Each morning as I stepped from the shower he blocked my way, the tug toy in his teeth. We did ten to fifteen reps. He usually won.
And then, sure enough, the problem went away like things do. I think it was Calvin Coolidge who said "If there's ten problems coming at you down the road, chances are nine will run into a ditch."
I am a real doctor, a board-certified neurologist who practiced every day for 30 years. I have had to retire.
After receiving my diagnosis in July, I couldn't quite admit it but at the tender age of 68, I was dying. I still felt young. I still hadn't made my millions. I still enjoyed what I did as a neurologist. Visit my old "Cybersuite" — it's like my memory attic now but there's a good headache questionnaire, a good translation of a book by Giacomo Casanova, and a good case against the death penalty and an extensive case against Electroconvulsive Therapy – ECT. Please visit Dr. John's Cybersuite.
Back to my Stage IV kidney cancer — and as another cancer patient, the writer Christopher Hitchens reminds us, there is no Stage V — carries a grim 5% five-year survival. Not so good.
My being a doctor had nothing to do with being lucky, but maybe sensible in choosing my primary care physician, Roxanne Fiscella, M.D.
She refers those who ask about alternatives in oncology to Michael Broffman, a counselor in Marin County.
Mr. Broffman, in turn, included Dr. Nagourney's lab, Rational Therapeutics, under the humble heading "tests."
And three days after my return to Northern California and my emergency admission to the hospital in Oakland, my cell phone rang. It was Dr. Nagourney. He already had results. I was on a morphine drip at the time but there is nothing hazy or distorted in my recollection of his words. He wasn't effusive but he didn't hide his satisfaction.
"Your cancer is resistant to most of the drugs we tested including the newest forms of therapy but it is sensitive to three drugs. You could take them together in low doses. You won't lose your hair."
The written report followed: "
…after mechanical and enzymatic degradation, 16 different drugs were tested for the induction of cell death."
The conclusion:
"Ex Vivo best regimen would be Cisplatin plus Gemcitabine plus Xeloda."
I loved that report. I kept it at my bedside.
I read it out loud to callers and waved it at the oncology nurses, the respiratory therapists, even the cleaning staff and of course the busy doctors.
I thought it was the best-ever lab report and not just because of the good news but the clarity and the personalization. Heck, I loved the choices of type and font.
And two weeks after beginning the regimen recommended by the EVA-PCD, (Ex Vivo – Programmed Cell Death) my chest x-ray was clearing dramatically and I was getting better and better and better.
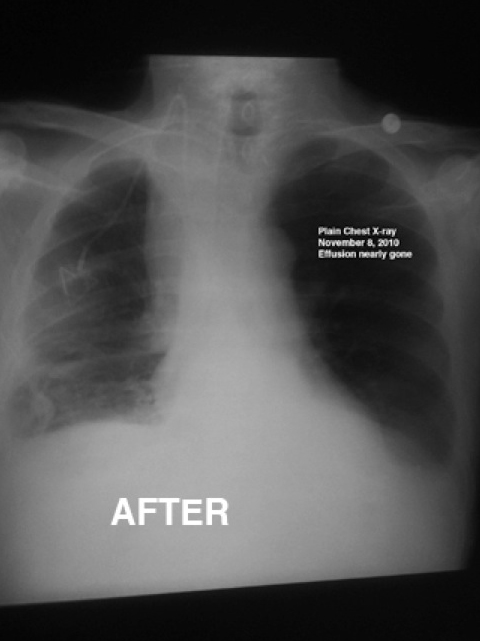
Finally, the tumor was surgically removed in its entirety in May and my last PET/CT scan in July was 100% negative for cancer.
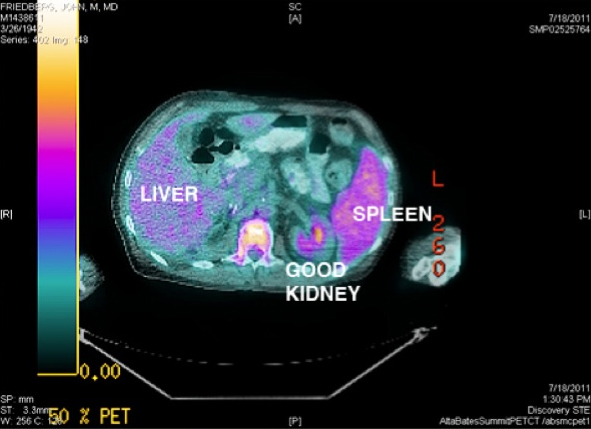
The urologist who got the bloody thing out in a strenuous six-hour operation, Dr. Robert Yan, gave me a hug.
Dr. Gary Cecchi, my oncologist and colleague, declared me in remission. He thought I could hold the chemotherapy for now. Cisplatin can cause kidney damage and I'm down to one.
Of course I had to call Dr. Nagourney who called me back at the tail end of his long day. He was not as sanguine: "The PET/CT only sees down to a centimeter. Hundreds of thousands of viable cancer cells can persist. Remember, if it comes back you'll probably die. This isn't mumblypeg we're dealing with here."
Dr. N had been right about everything else so far. As his office manager Shari Burt put it: "The only thing wrong with him is he's always right."
So I'm still on chemotherapy. I've had no adverse effects other than a neuropathy which has the advantage of allowing my new Yorkie puppy to teethe on my toes.
 Other than my life, I owe Dr. Nagourney the correct pronunciation of the word apoptosis, a beautiful word meaning "falling leaves" utterly ruined by my pronouncing both "p's" as in A POP tosis. Like POP-TOAST!
Other than my life, I owe Dr. Nagourney the correct pronunciation of the word apoptosis, a beautiful word meaning "falling leaves" utterly ruined by my pronouncing both "p's" as in A POP tosis. Like POP-TOAST!
It was the first thing he said to me when we met:
"Cancer cells don't grow too much, they die too little."
He explained how the programmed death of cells is apoptosis and a mutation starts the ball rolling toward cancer by taking out the gene for apoptosis.
Add a drug and look for dying leaves. No disrespect intended to Dr. Nagourney and a brave few but "The Test" would seem to be a no brainer.
And yet, neither Dr. Nagourney nor the test he does by any name used, most generically CSRA (chemosensitivity and resistance assay) which, following the lead of the best writer on the subject Ralph W. Moss shall be called simply "The Test" from here on, isn't so much as indexed in most texts and books.
In preparation for my talk this evening, I traveled to San Francisco's UC Medical School library where I hand-searched the indexes.
I also searched inside every relevant book on Amazon which allowed a search and it's a case of what the Germans call "death by silence" or the silent treatment.
Actually, it's worse than that. The Test is sharply attacked.
Just one month ago in August 2011, and before that in 2004, special panels were convened by the trade organization of all academic and private oncologists called ASCO — the American Society of Clinical Oncologists — for the express purpose of dismissing chemosensitivity and resistance assays as useless.
These critics ignore completely the newer, more common-sense methods nor do they mention or reference the fine published work by Drs. Nagourney, Weisenthal, and others. Over decades!
Wouldn't The Test save money all around? — for the insurers, the drug developers, the practicing doctors, and the patients by going for the best drug as determined by the Test?
Of course it would but who needs to save money when the National Cancer Institute alone disburses 5 billion dollars a year, mostly hunting the genomic snark while private charities contribute millions more.
The critics call for randomized controlled clinical trials (RCT's) and dismiss the robust positive correlations in prospective studies.
In theory randomized trials sound reasonable until you realize that this isn't a treatment we're talking about or a new drug. It's just a test!
It's a test like a blood culture or a CAT scan.
You don't test a test. For example, you don't take some peoples' temperatures and not others to find out if thermometers save lives.
All we ask of a test is that it be accurate. And The Test has proven accurate for both sensitivity and specificity time after time.
So who is smart enough to move this forward? We are. The patients. Above all, those whose lives have been saved by the Test. We are the real constituents.
Last November, when I was discharged from the hospital, I was blinking with the wonder of being alive. I was sure my story would be avidly seized on. After
all, I was a doctor whose ravaging kidney cancer melted away because of a combination of drugs which no one would have used had it not been for The Test.

You can imagine my astonishment when nobody whom I approached with my story — and I mean nobody — not the American Kidney Cancer Association, not the Dr. Oz Show, not two book agents, and not even Christopher Hitchens — nobody showed the slightest interest in a doctor plucked from the Big Kahuna. Turned around in two weeks. Cancer clearing like an antibiotic-treated pneumonia.
My Stanford oncologist who is no longer interested in hearing how I am doing but is being kept apprised regardless, reportedly told a kidney cancer patient that Dr. Nagourney's test had been tried by some and it doesn't work.
Underlying this defeatism is what is called therapeutic nihilism. Just as I did, the oncologists think they know the score: no significant improvement in the treatment of solid cancers as opposed to the leukemia's. Solid tumors are the big killers and there's been no improvement since the war on cancer was declared by Richard Nixon in 1971.
Even I knew that the bright claims for progress against cancer were eyewash. I thought I was a therapeutic nihilist: when it came to cancer nothing works, you're a goner.
But I had nothing on the authorities.
In my hospital library, in the largest shiniest cancer book on the shelf, titled simply Oncology, 2008 Edition, Vincent T. DeVita Jr. Editor, there is, on page 1172, this chilling sentence: "Chemotherapy currently has little or no role in the treatment of metastatic RCC."
Now that's nihilism.
What a weight off the soul to hear Dr. Nagourney say at the recent TedX convention: "I kill cancer."
Hope, or as Emily Dickinson calls it "the thing with feathers" — flutters.
I'd love to hear the taboo word "cure" but I'll settle for an indefinite death sentence like everyone else alive, every sentient being, and enjoy each moment and spread the word about The Test and its potential for saving and improving the quality of our lives.
Dr. Nagourney wonders rhetorically what he has to do to get noticed — catch bullets in his teeth? Hey, that's pretty much my trick, my Close Call.
For me it's been one more year of life so far. I swim, I work out, I housebreak a puppy, I look forward to another season of snowboarding.
And I try not to die because, to quote the late great Jack Lalane, "It would spoil my reputation."
Thank you.
PS: I lost my seven year old wonderdog Buddy just as I was preparing this talk. He was attacked and killed out of the blue by a "rescue" Rhodesian Ridgeback.
I got through this past year in part thanks to him and in part for him. We knew each other. We trusted each other. He is deeply missed.

PPS: Watch my talk on YouTube below.
PART 1
PART 2
Chapter 8: Tribute to Buddy
As a tribute to my Yorkshire Terrier, killed in his prime by a vicious Rhodesian Ridgeback "rescue dog," I dedicate this last chapter and indeed my whole book.
I couldn't have done it without him. His image was a "skin" on my cellphone and I would gaze at it when I couldn't do anything else.
And he was totally there for me when I got out of six weeks in the hospital. I couldn't even throw his ball down the hill but he didn't care.
I never expected him to go before me, my brave little boy always so careful and polite. He got ambushed by an immense animal named "Kweli."
Buddy and I have more than 90 videos on Youtube but this one from 2008 when he was 4 is my favorite.
Note he didn't need treats to do his tricks.
Mostly he did it for the fun and love we shared together and, of course, with hundreds of patients over the years as well as our passionately attended meetup group, Yorkies and Friends.
He went with me twice to Hawaii, snowboarded KT22 at Squaw, sired 12 good children and was, overall, a very lucky dog.
He will be missed forever.